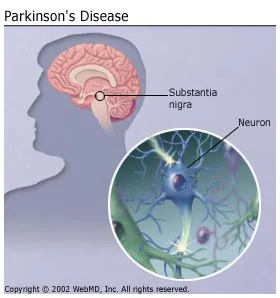
When cells in the brain are damaged and die, for instance by stroke, there will be no repair or scar formation for those cells. The brain tissue will undergo liquefactive necrosis, and a rim of gliosis will form around the damaged area. Apart from a small amount in the blood vessels, there is no collagen or fibroblasts in the brain. A scar is formed by fibroblasts producing collagen to repair an area, which will later contract. If scars did form in the brain, the contraction would cause even more damage.
Around the edge of necrosis, astrocytes proliferate. These cells extend processes, and form a delicate rim of gliosis around the margin of damage. The empty space left by brain tissue fills up with cerebrospinal fluid.
Brain injury will commonly be accompanied by acute swelling, which impairs function in brain tissue that remains alive. Resolution of swelling is an important factor for the individual's function to improve. The greatest factor in functional recovery after brain injury comes from the brain's ability to learn, called neuroplasticity. After injury, neuroplasticity allows intact areas of the brain to adapt and attempt to compensate for damaged parts of the brain. Although axons and the peripheral nervous system in the developing brain can regenerate, they cannot in the adult brain. This is partly because of factors produced by cells in the brain that inhibit this regeneration. Dendrites, however, will develop from intact axons, as part of the neuroplasticity process. After severe brain injury, improvement in function related to neuroplasticity is unlikely to occur without help from health professionals skilled in rehabilitation.
In 1990 Dr. Richard Neubauer proved that these idling neurons can exist for years. In a groundbreaking experiment Dr. Neubauer performed hyperbaric oxygen therapy on a woman paralyzed for 14 years after a stroke. He found that after just one treatment, blood flow increased in the idling neurons surrounding her damaged tissue.
Traditionally, Hyperbaric Oxygen Therapy (HBOT) has been used as a technique to heal chronic wounds by rebuilding tissue. Patients enter a chamber and are exposed to high volumes of oxygen at great pressure. HBOT overcomes “stunned” cells, allowing them to function more normally again. In addition, it was recently proven that HBOT primarily affects genes in our cells that code for growth and repair hormones that inhibit inflammation and cell death.
For stroke survivors, HBOT reactivates the idling neurons, stimulates growth of new blood vessels, prevents cell death, and improves neurological function. HBOT has also been shown to cause the release of stem cells from our bone marrow into our circulation, where they are distributed throughout the body.
In recent years HBOT therapy has gained popularity as a treatment method for various traumatic brain injuries. Dr. Paul Harch, in New Orleans, treated a diver demented from brain decompression sickness. Brain decompression sickness is the quintessential example of HBOT in stroke: tiny bubbles passing through tiny blood vessels, damaging the blood vessels and causing thousands to millions of tiny spherical strokes or wounds in the brain. In two months of treatment the diver had improved cognitive, neurological, brain blood flow, and quality of life.
Successful treatments with HBOT was seen in other divers, patients with chronic stroke syndromes, and veterans returning with traumatic brain injuries and post-traumatic stress disorder. The amount of benefit HBOT can provide a stroke survivor depends on many factors.
- The size of the stroke
- The length of time since the stroke
- The area of the brain involved
- The type of stroke
- Whether or not the patient received a clot-dissolving drug
Existing evidence suggests that HBOT is the most beneficial when started as soon after stroke as possible.
There are risks associated with HBOT, similar to some diving disorders. Pressure changes can cause a "squeeze" or barotrauma in the tissues surrounding trapped air inside the body, such as the lungs, behind the eardrum, inside paranasal sinuses, or trapped underneath dental fillings. Breathing high-pressure oxygen may cause oxygen toxicity. Temporarily blurred vision can be caused by swelling of the lens, which usually resolves in two to four weeks.
Patients inside the chamber may notice discomfort inside their ears as a pressure difference develops between their middle ear and the chamber atmosphere. This can be relieved by the Valsalva maneuver or by "jaw wiggling". As the pressure increases further, mist may form in the air inside the chamber and the air may become warm. Increased pressure may also cause ear drums to rupture, resulting in severe pain. To reduce the pressure, a valve is opened to allow air out of the chamber. As the pressure falls, the patient’s ears may "squeak" as the pressure inside the ear equalizes with the chamber. The temperature in the chamber will fall. The speed of pressurization and de-pressurization can be adjusted to each patient's needs.
- Patients should not undergo HBO therapy if they are taking or have recently taken the following drugs: Doxorubicin (Adriamycin) – A chemotherapeutic drug. Cisplatin – Also a chemotherapeutic drug.
- Disulfiram (Antabuse) – Used in the treatment of alcoholism.
- Mafenide acetate (Sulfamylon) – Suppresses bacterial infections in burn wounds
Evidence in a 2005 systematic review of the evidence for HBOT in the treatment of stroke showed no benefit to the treatment, though the generalizability of the finding was limited due to the wide variety in stage and type of stroke, and the treatment given. Good quality studies were recommended to determine if HBOT provides any benefit in stroke. Another review that examined the effectiveness of HBOT in acute stroke. It found no evidence that HBOT improved clinical outcomes at 6 months, but further study was recommended.
Despite lack of evidence, research from health pioneer (and former ANH-USA board member) Dr. Paul G. Harch published in the Journal of Neurotrauma indicates that hyperbaric oxygen therapy, or HBOT, is able to dramatically help veterans with post-concussion syndrome (a form of traumatic brain injury) and post-traumatic stress disorder (PTSD). Dr. Harch is an associate clinical professor of medicine at Louisiana State University in New Orleans.
Since January 2007, ANH-USA has been bringing attention to a project to have veterans treated with HBOT. In HBOT, the patient is put in a hyperbaric oxygen chamber, which saturates the tissues with twelve times more oxygen than can be absorbed by breathing. This greatly enhances the body’s own healing process.
According to Dr. Harch’s new study, even three years after the vets sustained brain injury, one month of HBOT was able to induce improvements in brain blood flow, cognition, symptoms, and quality of life, while the veterans experienced fewer suicidal thoughts. Specifically, improvements were seen in 92% of vets experiencing short-term memory problems, 87% of those complaining of headaches, 93% of those with cognitive deficits, 75% with sleep disruption, and 93% with depression. There were also improvements in irritability, mood swings, impulsivity, balance, motor function, IQ, and blood flow in the brain, as well as the reduction in PTSD symptoms and suicidal thoughts. And there was a reduction in—or complete elimination of—psychoactive and narcotic prescription medication usage in 64% of those previously prescribed the medication.
Besides the uses of a Hyperbaric chamber to avoid decompression sickness, there are people on both sides of the fence who are either promoting or debunking the healing properties of pressurised oxygen supply. The risks of Hyperbaric Oxygen Therapy might be too much for those whose medication counteracts the healing effects. Other illnesses such as Cardiac disease or Emphysema with CO2 retention have negative results with HBOT. This narrow field of users and complications of oxygen toxicity reduces its chances of being a confirmed method of healing. Despite the debunking or the lack of FDA approval there is a growing acceptance for people with cerebral palsy, stroke victims,encephalitis or PTSD not to mention a few other illnesses who claim to have success.
Oxygen therapy in this pressurized configuration might not be the ideal cure, but perhaps oxygenating the blood supply could offer an alternative. Only recently scientists created micro-particles into fat which oxygenates the blood safely without embolisms. If the goal of HBOT is to oxygenate the blood, it could theoretically be a sound method to minimalize the risk of oxygen toxicity by way of micro-particles. Curing brain damage is relatively a new science, while trials are still carrying on, there will be critics from both sides that will argue their cases. In this case I am hopeful there will be several different methods including micro particles that will establish neural repairs of any kind...